Pet-owners want to know: Why is my dog licking so much that a sore spot forms?
It’s a lot like kids who suck their thumb — once the habit starts, it’s hard to break. Here’s what you need to know about causes and treatment.
A dog’s list of annoying habits can often be endless. Obsessive itching, licking, scratching, urinating on your favorite rug, jumping up on people— endless. Similar habits, such as dog licking that is taken to self-harm levels, that results in the dog developing sores called lick granulomas.
Maybe you’ve seen this: a raised, red sore on a front leg that your dog licks at obsessively. Or perhaps you never seen your dog lick, but the sore is there all the same.
Chances are you told your dog to stop, so they learned to become secretive about licking. Well, these sores are surprisingly common.
Why your dog is constantly licking one spot
Dogs aren’t much different from us. Once the habit starts, it’s hard to break.
The reason is that the dog licking releases feel-good hormones called endorphins. The dog licks, it feels good, and the dog doesn’t want to stop licking.
You may hear your vet refer to the condition as acral lick dermatitis, or ALD, where dogs are licking their legs so much that sores developed.
Studies have shown that when nature’s own morphine-like substances — the endorphins — are involved in ALD, because affected dogs’ self-licking behavior decreased dramatically when the dogs were treated with endorphin antagonists. Since endorphins are released when stress arises, it can be confirmed that licking appears in situations where stress is involved.
Possible Health-Related Causes of the Licking
For most dogs, the habit starts with a trigger in the form of an itch, ache or infection.
It may be that the dog has arthritis or an allergy, and rather than lick the specific spot, the dog chooses a comfortable place to lick — which is often a forearm or paw.
Common triggers:
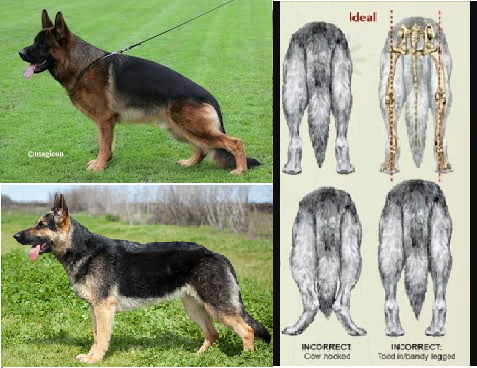
Arthritis
Parasitic infection that causes a general itch
A bacterial skin infection
Ringworm
Skin allergies triggering an itch
More than half of dogs with acral lick dermatitis are suspected to have concurrent fear- or anxiety-based conditions or both (e.g., separation anxiety, noise phobia, anxiety-related aggression).
The Derma Dilemma
The problem is that a veterinarian cannot give the owner a specific recipe for a cure. The skin lesions will heal slightly, almost seem like they are going to heal, but then overnight (or during the day while left alone) the lick granuloma is activated by the dog licking the area raw once again.
Even worse, some dogs will simply switch to licking the other leg if you restrict their ability to lick the first leg by wrapping it in a cast, creating an even more annoying problem—now there are 2 lick granulomas!
Does Your Dog Do This? If So, Act Quickly.
If your dog starts to lick obsessively, seek the help of your veterinarian. Getting to the bottom of the cause, and early treatment, is the best way to stop the problem from becoming ingrained.
Alongside treating the lick granuloma, your vet may want to run tests to investigate any underlying problems.
Treatment of Lick Granulomas / Sore Spots in Dogs
Think of this as a 2-pronged attack: tackling both the sores and the underlying cause.
Lick granulomas are frustrating because even with successful treatment, the dog is likely to relapse. To stand any chances of long-term success, therapy must continue for at least 4 weeks after the symptoms have ceased.
Treating the sores:
Antibiotics or antifungals
Local anesthetic creams
Anti-inflammatory medications (to reduce the skin tingle)
Bandages or an Elizabethan collar (“cone of shame”)
Mood-modifying drugs
Your vet may try one or a combination of the treatments above.
Frustratingly, putting an Elizabethan collar on doesn’t work well because as soon as it is removed, the licking starts again and the dog will activate the lesion all over again.
Addressing the underlying triggers:
The first step is to find out what they are. This could mean blood tests, skin biopsies or radiographs.
In the case of allergies, starting the dog on a hypoallergenic diet is a great idea, as is testing for environmental allergens.
Regular parasite treatments against fleas and mites are crucial to keep parasitic itches at bay.
Ultimately, to find the right solution for your dog, speak with your vet.
Hear From Us Again
Don't forget to subscribe to our email newsletter for more recipes, articles, and clinic updates delivered straight to your e-mail inbox.
Related Categories: