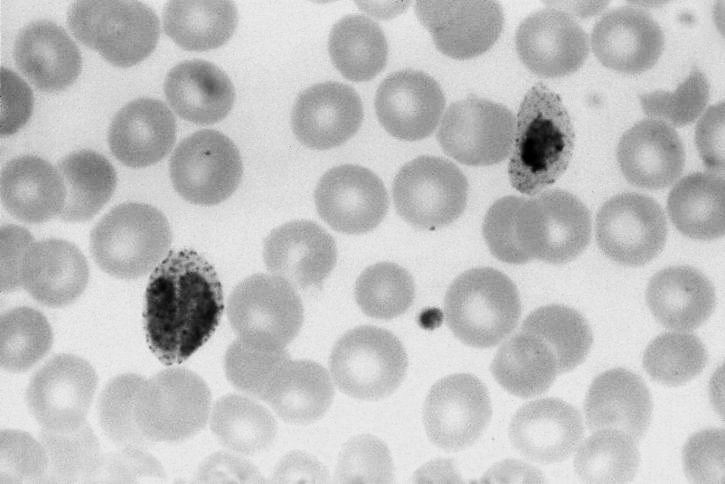
What is Toxoplasmosis?
Toxoplasmosis is an infection caused by a microscopic parasite called Toxoplasma gondii. More than 60 million people in the United States carry the Toxoplasma parasite. Toxoplasmosis can cause severe illness in infants infected before birth (When their mothers are newly infected during pregnancy), or in persons with a weakened immune system.
What role do cats play in the spread of Toxoplasmosis?
Cats get Toxoplasma infection by eating infected birds, rodents, and other small animals, or anything contaminated with feces from another cat that is shedding the microscopic parasite in it's feces. After a cat has been infected, it can shed the parasite for up to two weeks. The parasite becomes infective one to five days after it is passed in the feces of the cat. The parasite can live in the environment for many months and contaminate soil, water, fruits and vegetables, sandboxes, grass where animals graze for food, litter boxes, or any place where an infected cat may have defecated.
How are people infected with Toxoplasma?
There are several ways in which people may become infected with toxoplasosis.
Eating food, drinking water, or accidentially swallowing soil that has been contaminated with infected cat feces (think: homegrown produce that feral cats may have access to!).
Eating raw or undercooked meat from animals (especially pigs, lamb, or wild game) that have been infected with Toxoplasma.
Directly from a pregnant woman to her unborn child when the mother becomes infected with Toxoplasma just before or during pregnancy.
What are the symptoms of toxoplasmosis?
Individuals with a healthy immune system:
Most people who become infected with Toxoplasma do not know it and have no symptoms. However, when illness occurs, it is usually mild. Some may feel like they have the “flu”, with swollen lymph glands, or muscle aches and pains that last for several weeks or more. Although rare, eye disease may also occur.
Individuals with weakened immune systems:
People with weakened immune systems may experience severe symptoms. The most common symptoms in people with HIV infection are headache, confusion, and fever. Other symptoms include seizures, poor coordination, and nausea or vomiting.
Infants infected before birth:
Most infants infected with Toxoplasma before birth show no symptoms at birth. However, many are likely to develop symptoms later in life. These include vision loss, mental disability, and seizures.
How can I protect myself from toxoplasmosis?
Several steps can be taken to protect yourself and others from toxoplasmosis.
Change your cat litter boxes daily. Toxoplasma takes more than one day to become infectious. If you are pregnant or have a weakened immune system, ask someone else to change the litter box. If this is not possible, wear disposable gloves and wash your hands thoroughly with soap and water afterward.
Cover any outdoor sandboxes when not in use to keep cats from defecating in them.
Avoid adopting stray cats, especially kittens, off the streets (go through an agency such as our local Cat Depot to assure a happy & healthy stray). Younger cats are more likely to be releasing Toxoplasma in their feces.
Do not eat undercooked meat. Cook meat until the internal temperature reaches 160° Fahrenheit.
Wash all kitchen supplies (such as knives and cutting boards) that have been in contact with raw meat.
If you have a weakened immune system, it is important to talk to your health care provider about getting a blood test to determine if you have been infected with Toxoplasma.
How can I protect my cat from toxoplasmosis?
Protecting your cat from toxoplasmosis may also help to protect you from toxoplasmosis.
Feed your cat commercial dry or canned food.
Never feed cats raw meat because this can be a source of Toxoplasma infection.
Keep indoor cats indoors so they do not become infected by eating small animals.
Do I have to get rid of my cat?
No, you do not have to give up your cat. Owning a cat does not mean you will be infected with the parasite. It is unlikely that you would be exposed to the parasite by touching the infected cat, because cats usually do not carry the parasite on their fur coat. In addition, cats kept indoors (that do not hunt prey or feed on raw meat) are not likely to be infected with Toxoplasma. But, if you are pregnant, or have a weakened immune system, it is important to protect yourself from infection.
Can toxoplasmosis be treated?
Yes, most certainly. There is a treatment for toxoplasmosis. In an otherwise healthy person, mild symptoms typically go away within several weeks to months, and treatment is not needed. However, treatment may be recommended for an otherwise healthy person with eye disease due to toxoplasmosis. A woman who becomes infected during pregnancy can be treated with medication that may protect her unborn child from toxoplasmosis. Mother and baby should be monitored closely during pregnancy and post-birth.
Hear From Us Again
Don't forget to subscribe to our email newsletter for more recipes, articles, and clinic updates delivered straight to your e-mail inbox.
Related Categories: